An intrathecal pain pump is a surgically implanted medical device that delivers pain medication directly to the intrathecal space surrounding the spinal cord.
By bypassing the digestive system and bloodstream, this method allows a much smaller dose of medication to be delivered with greater efficiency and fewer systemic side effects.
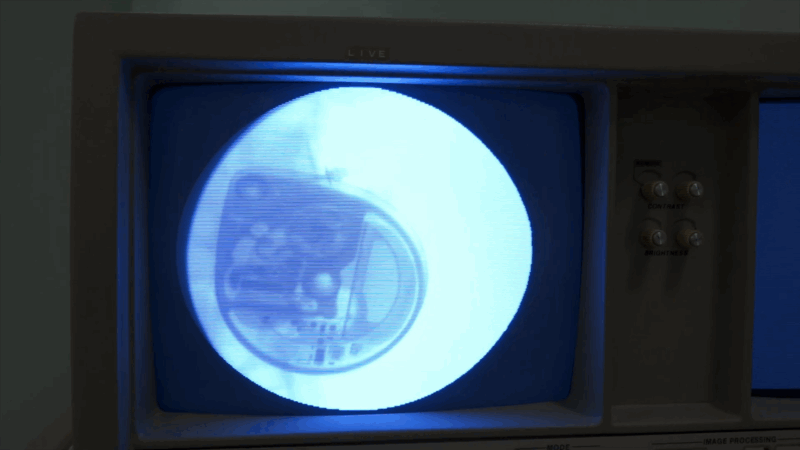
The pump, typically about the size of a hockey puck, is implanted under the skin, usually in the lower abdomen.
A catheter connected to the pump runs under the skin to the spinal canal, where the medication is released directly to the fluid around the spinal cord.
This area contains pain receptors, including opioid receptors, that respond quickly and effectively to medication, often halting pain signals before they reach the brain.
This method of drug delivery is particularly useful for individuals with severe chronic pain or spasticity that has not responded well to oral medications or other conventional treatments.
Why Is an Intrathecal Pain Pump Used?
While an intrathecal pain pump does not cure the underlying cause of pain, it can greatly improve the quality of life for individuals who struggle with ongoing discomfort, limited mobility, or the side effects of high-dose oral medications.
Conditions Commonly Treated with Intrathecal Pain Pumps
For these and other conditions, a pain pump may offer relief when other treatments have failed or caused intolerable side effects.
Intrathecal Pain Pump Trial: Determining Candidacy

Before committing to permanent implantation of an intrathecal pain pump, patients typically undergo a trial phase to determine if this method of pain management will be effective for their specific condition. This step is critical for identifying those who are likely to benefit from the device and ensuring a personalized, successful treatment plan.
During the trial, a physician administers a single dose of pain medication directly into the spinal fluid via a temporary catheter or injection. This approach mimics the way medication would be delivered by a permanent pump. The patient’s pain levels are closely monitored both before and after the administration to evaluate the response.
If the patient experiences a reduction in pain of 50% or more, the trial is considered successful. In such cases, the individual is deemed a suitable candidate for permanent pump implantation. This process helps to minimize unnecessary surgeries and ensures that the implanted device will likely provide meaningful relief.
What to Expect Before, During, and After the Procedure
View this post on Instagram
Preoperative Preparation
In preparation for the surgical implantation of an intrathecal pain pump, patients undergo several important assessments. First, presurgical testing is conducted to evaluate the patient’s overall health and to ensure they are medically fit for surgery. This may include blood work, imaging, and other standard preoperative evaluations.
A psychological assessment is often required to determine whether psychological or emotional factors may be contributing to the perception of pain. This is not only a standard precaution but also an important part of tailoring the pain management approach to each individual’s needs.
Patients also meet with an anesthesiologist who will review the planned sedation method, go over any potential risks or side effects, and answer any questions the patient may have. In most cases, the procedure is performed under local anesthesia with sedation, allowing the patient to remain relaxed but not fully unconscious.
However, general anesthesia may be used if clinically indicated or based on patient preference and complexity of the surgery.
In the hours leading up to surgery, patients are instructed to refrain from eating or drinking after midnight. Upon arrival at the surgical facility, an intravenous (IV) line is inserted to allow for the administration of fluids, sedatives, and other necessary medications before and during the procedure.
During the Procedure

Once sedation takes effect, the patient is positioned on their side. The back and lower abdomen are cleaned and shaved to reduce the risk of infection. The surgical process includes:
- Catheter Placement – A small incision is made in the lower back. A catheter is inserted into the intrathecal space of the spinal canal to deliver the medication.
- Pump Insertion – A second incision is made in the lower abdomen, below the waistline, where the pump will be implanted.
- Connecting the System – A subcutaneous tunnel is created for the catheter to travel from the spine around the side of the torso to the pump. Once the catheter is connected to the pump, the device is carefully secured in place under the skin, ensuring it doesn’t protrude or cause discomfort.
- Closing the Incisions – Both incisions are closed using sutures or surgical staples, and sterile dressings are applied.
Postoperative Recovery
After surgery, patients are moved to a recovery area, where vital signs and surgical sites are closely monitored.
Most patients can return home within a day, depending on individual health and recovery speed.
Recovery Guidelines Include:
Benefits of an Intrathecal Pain Pump
@dr.mikesaysfnp #clinicalanswers #painmanagement #fyp #drmikesays ♬ original sound – DrMikeSays Media,LLC
There are several compelling reasons why intrathecal pumps are preferred over oral pain medications in certain patients:
1. Lower Dosage Requirements
The pump delivers medication directly to the spinal cord, allowing for much smaller doses compared to oral routes. This not only increases effectiveness but also reduces the risk of tolerance and side effects.
2. Fewer Systemic Side Effects
Common side effects of oral opioids, such as nausea, drowsiness, and constipation, are often reduced or eliminated with spinal drug delivery.
However, recurrence of nausea can sometimes occur following procedures like ventriculoperitoneal shunt replacement, which may complicate pain management in certain patients.
3. Lower Risk of Opioid Dependency
Because such a small amount of opioid is needed, the risk of addiction and dependence is significantly lower compared to high-dose oral opioid therapy.
4. Programmable and Customizable
Pain pumps can be programmed to release medication at consistent intervals or adjusted to provide additional doses at specific times (with a physician’s input). This allows tailored pain management to meet the patient’s needs.
5. Improved Quality of Life
Patients who suffer from debilitating pain may find that the pain pump enables them to reduce or eliminate oral medications, regain functionality, and return to activities they previously avoided.
Is an Intrathecal Pain Pump Right for You?
An intrathecal pain pump can offer profound relief for certain patients with chronic pain or spasticity, especially when conventional treatments have proven inadequate.
However, not all individuals are suitable candidates. Factors such as medical history, current medications, psychological profile, and the type of pain being treated all play a role in determining whether this solution is appropriate.
Final Thoughts
Intrathecal pain pump placement is a powerful and targeted treatment for managing chronic, severe pain and neurological muscle spasticity. While it involves surgery and lifelong monitoring, many patients find it significantly improves their comfort, functionality, and overall quality of life.
When used properly, this technology allows for pain relief with fewer risks and side effects than traditional oral medications, offering a safer long-term option for pain control.
If you or someone you care for is living with chronic pain that has not responded to medication, physical therapy, or previous surgery, intrathecal drug delivery systems may offer the hope and relief you’ve been seeking.
