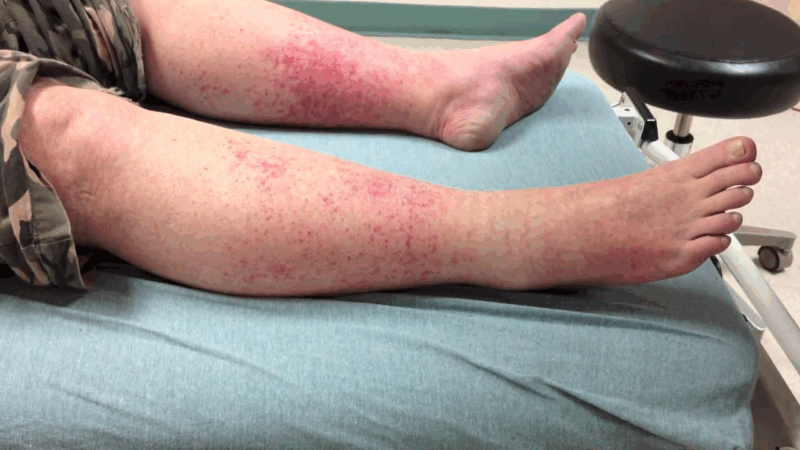
The so-called “Disney rash” is not a condition exclusive to amusement parks, but it got its nickname because many people report developing a red, itchy rash on their lower legs after spending long days walking at Disney theme parks.
Medically, this condition is known as exercise-induced vasculitis (EIV) or golfer’s vasculitis, and it’s a form of small vessel inflammation triggered by extended walking or standing in warm temperatures.
The Disney rash is not caused by an allergy, infection, or contact with chemicals, but by a physical stress response in the superficial blood vessels of the skin, particularly in the lower legs. The most affected individuals tend to be middle-aged or older adults, especially women over 50, although younger people can experience it too.
What makes this condition unique is that it often appears in healthy individuals who are not otherwise prone to skin problems, and the symptoms usually resolve on their own without treatment—though they can look alarming and feel uncomfortable.
What Causes the Disney Rash?
The root cause of the Disney rash lies in superficial blood vessel dysfunction, triggered by heat and increased hydrostatic pressure in the legs. The following mechanisms are involved:
1. Vascular Dilation and Gravity-Induced Pressure
When a person walks or stands for a prolonged period—especially in high temperatures—blood pools in the lower extremities, increasing capillary pressure. This pressure causes capillary leakage, where small blood vessels allow plasma and red blood cells to escape into the surrounding tissue. The result: patches of inflammation, redness, and petechiae (tiny red dots).
2. Heat-Induced Capillary Fragility
Exposure to heat makes blood vessels more permeable and fragile. In some people, especially those with naturally sensitive skin or age-related vascular changes, this can cause capillaries to rupture easily, leading to redness, swelling, and itching.
3. Immune Response to Stress
Exercise-induced vasculitis may also involve a mild immune reaction, where the body responds to the vascular leakage by releasing inflammatory mediators, though not to the level of autoimmune vasculitis seen in systemic disease.
It is not caused by allergens, sunscreens, soaps, or park chemicals—though these can sometimes worsen the irritation once the rash appears.
Who Is Most at Risk?
View this post on Instagram
Although the Disney rash (exercise-induced vasculitis) can occur in virtually anyone, especially under intense environmental stress, certain populations exhibit a notably higher risk profile. This pattern emerges clearly across both anecdotal accounts and dermatological case series.
1. Individuals Over Age 50
With age, blood vessels naturally become less elastic and more susceptible to damage under thermal or gravitational stress. Older adults also have a higher prevalence of venous insufficiency, a known contributor to superficial capillary leakage.
As a result, even moderate exertion in the heat can cause microvascular inflammation in the lower extremities.
2. Women
Exercise-induced vasculitis disproportionately affects women, particularly postmenopausal women. Hormonal changes may affect vascular reactivity and skin integrity, though precise mechanisms remain unclear.
Women are also more likely to wear tight-fitting footwear or compression garments that can localize pressure and exacerbate the rash pattern.
3. People With Venous Insufficiency or Varicose Veins
Chronic venous congestion leads to increased hydrostatic pressure in the lower limbs, a key trigger for capillary rupture and inflammatory response.
Individuals with visible varicosities or a history of edema in the legs are particularly vulnerable during prolonged standing or walking.
4. Those Exposed to Long Walking Durations
The Disney rash is a kind of blood vessel inflammation called vasculitis that affects the lower parts of the legs after you perform strenuous exercise or activity for a long time, especially in warm weather. https://t.co/YgyqQF1w2L pic.twitter.com/R1VPwv6Eju
— WebMD (@WebMD) April 22, 2024
Whether it’s hours spent exploring a theme park or completing a long hike, duration plays a central role. Sustained ambulation increases peripheral blood pooling, worsens fluid pressure in lower limb vessels, and predisposes the skin to inflammation.
5. Exposure to Heat and Humidity
High temperatures dilate blood vessels, increasing permeability and the risk of leakage into surrounding tissue. When combined with sweat retention or tight clothing, the risk of EIV is further amplified.
6. Use of Socks or Tight Shoes
The rash often spares the area under socks due to compression. However, these same garments can cause localized friction and heat buildup, contributing to the irregular appearance and discomfort associated with the condition.
Importantly, this condition may arise even in completely healthy individuals without any prior dermatologic or vascular history, particularly under the right mix of temperature, stress, and exertion.
Clinical Presentation and Diagnosis

The diagnosis of exercise-induced vasculitis is typically clinical, meaning it is made based on the patient’s physical presentation and activity history. Laboratory testing is unnecessary in most cases unless systemic involvement or differential diagnosis is a concern.
Typical Skin Findings
Key Differential Diagnoses
Condition
Distinguishing Feature
Allergic Contact Dermatitis
Itchy, blistering rash with a defined exposure pattern
Heat Rash (Miliaria)
Typically affects trunk or upper body; linked to sweat ducts
Stasis Dermatitis
Chronic with scaling, hyperpigmentation, and edema
Cellulitis
Painful, swollen, warm, and usually unilateral with fever
Purpura Simplex
Localized bruising from minor trauma; not activity-triggered
How Common Is the Disney Rash?
@nat_tello It happens to many of us! Mine usually burn so much. I wore light pants to protect me from burning even more. It was gone in about 2/3 days! The cold compress gives such a relief! Also cold water while showering. 👏🏻 Consult a doctor if rash is severe and does not go away with home treatment. #disneyrash #themeparks #selfcare #disney #orlando #florida ♬ Disco Inferno (Edit) – The Trammps
While large-scale prevalence data is limited, EIV is underreported but not uncommon. Dermatology clinics often encounter patients with this condition during the warmer months.
One case series published in Clinical Dermatology (2001) documented more than 30 individuals who developed the condition after long summer walks. Many were misdiagnosed initially with contact dermatitis or cellulitis.
Groups frequently affected include:
Treatment: What Helps and What Doesn’t
Exercise-induced vasculitis is typically self-limiting, and no prescription medication is needed in most cases. The primary goal is symptom management and avoiding further aggravation.
Treatment Method
Purpose
Cool Compresses
Reduce inflammation and skin temperature
Leg Elevation
Encourages venous return and reduces swelling
Antihistamines (oral)
Controls itching and histamine-driven inflammation
Topical Corticosteroids
Minimizes localized inflammation in more severe rashes
Avoid Heat and Strain
Prevents recurrence and aids in symptom resolution
Antibiotics, alcohol, or antifungal creams should not be used unless a secondary infection is present. Inappropriately treating the rash as an infection can delay proper management.
Preventive Measures That Work
Preventing recurrence centers on thermal regulation, vascular support, and activity modification:
In individuals prone to recurrence, pre-walk cooling strategies (such as ice packs or leg elevation before activity) may also help.
Conclusion
The Disney rash is a visible but harmless dermatological event triggered by common environmental and physical stressors. Recognizing its pattern is crucial for avoiding unnecessary worry or medical interventions.
Interestingly, some early symptoms of meningitis—like skin rashes—can appear similar, which makes accurate identification essential in more serious contexts.
Most importantly, it underscores the need for heat management and vascular support, especially among older adults engaging in physical activity in hot climates.
Education and preventive strategies can drastically reduce recurrence. And while it may go by a lighthearted nickname, the physiological dynamics behind the Disney rash offer real insight into how our bodies respond to heat, gravity, and motion in subtle but meaningful ways.
