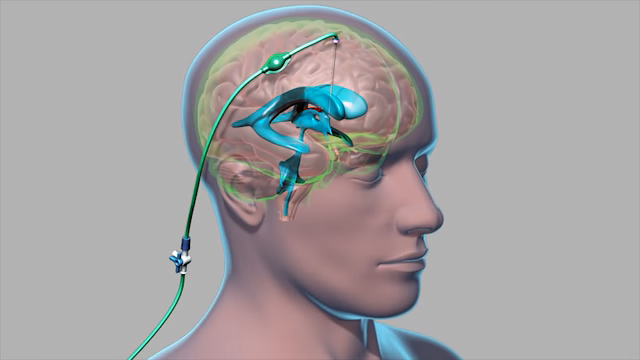
A ventriculoperitoneal (VP) shunt is a medical device used to treat hydrocephalus, a condition in which cerebrospinal fluid (CSF) accumulates in the brain’s ventricles, increasing pressure inside the skull.
Left untreated, this pressure can lead to headaches, nausea, balance issues, visual disturbances, cognitive decline, and other neurological problems.
The VP shunt system diverts excess CSF from the brain to the peritoneal cavity in the abdomen, where it can be absorbed naturally by the body.
This shunting relieves intracranial pressure and helps reduce the symptoms of hydrocephalus. The system generally consists of three parts:
Overview
View this post on Instagram
Over time, VP shunts may fail or become less effective, requiring replacement surgery.
A ventriculoperitoneal shunt replacement is a surgical procedure that involves removing part or all of the existing shunt system and installing a new one.
This may be necessary due to mechanical malfunction, infection, over- or under-drainage, or changes in a patient’s condition.
Although some shunts last for several years, studies show that many need replacement or revision after about six years.
According to data from the Johns Hopkins Institute, while some patients (about 10%) show rapid improvement shortly after shunt placement, they may later experience reduced long-term benefits, often due to complications that require further intervention.
When Is a Shunt Replacement Necessary?
These include:
1. Blockages or Obstructions
Shunt systems can become clogged by debris, tissue, or blood, preventing the proper flow of cerebrospinal fluid.
Blockages may occur in either the ventricular or distal catheter or in the valve itself.
These blockages can often be corrected through surgery and, if addressed quickly, typically do not cause long-term damage.
2. Overdrainage or Underdrainage
Shunts are designed to regulate the amount of CSF that is drained, but malfunctions can cause them to drain too much or too little.
Overdrainage can lead to conditions like subdural hematomas or slit ventricle syndrome, while underdrainage can cause symptoms of hydrocephalus to return.
3. Infection

Infection is a serious complication and may occur at the surgical incision site, along the catheter path, or within the central nervous system.
Meningitis, an infection of the brain’s protective membranes, can also result from shunt-related complications.
Warning signs include:
4. Symptom Recurrence
If symptoms of hydrocephalus—such as headaches, gait instability, nausea, or visual disturbances—return after a period of stability, it may indicate that the shunt is no longer functioning correctly.
Emergency evaluation and possibly surgical revision may be required.
How Is It Performed?
Ventriculoperitoneal (VP) shunt placement is a crucial surgical intervention aimed at treating hydrocephalus, a condition characterized by excessive accumulation of cerebrospinal fluid (CSF) within the ventricular system of the brain. This procedure involves inserting a catheter…
— Raffaele Di Giacomo, PhD (@sciqst) July 23, 2024
VP shunt replacement surgery is generally performed under general anesthesia in a hospital setting and takes about 90 minutes on average.
The procedure may involve partial or complete replacement of the existing system, depending on the location and nature of the issue.
Preoperative Preparation
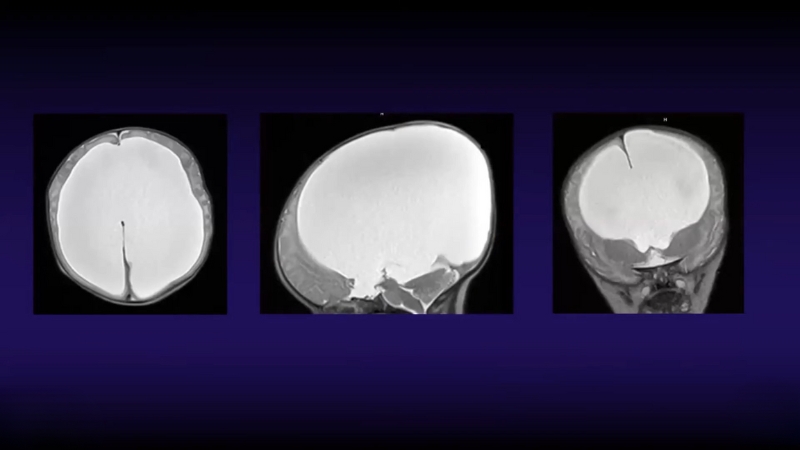
Before surgery, patients undergo imaging tests such as MRI or CT scans to evaluate the current condition of the shunt and brain ventricles.
Blood work and infection screening are also performed to ensure the patient is fit for surgery.
Surgical Steps
The procedure follows these general steps:
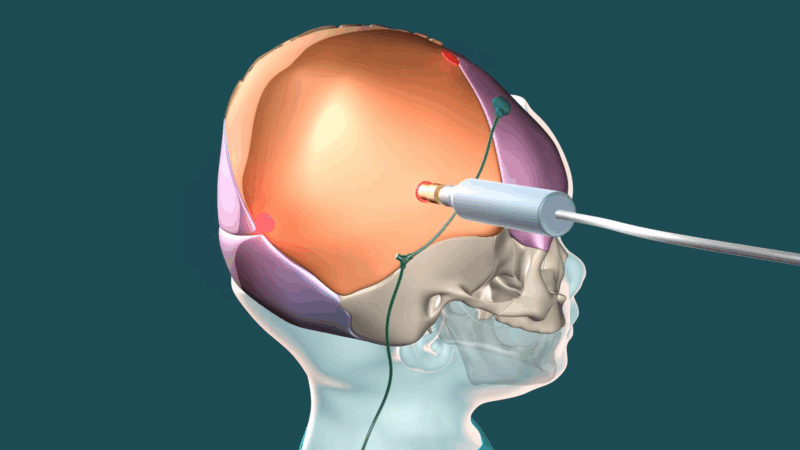
- Scalp Preparation and Incision A portion of the scalp—usually at the top or back of the head—is shaved and prepped. The surgeon makes a small incision behind the ear, where the valve is usually located.
- Abdominal Incision A second incision is made in the abdomen, where the distal catheter terminates. This allows access to the peritoneal cavity, where the catheter drains CSF.
- Accessing the Brain Ventricles: A small hole is drilled into the skull to remove the malfunctioning ventricular catheter. An endoscope may be used for direct visualization of the brain’s ventricles, enhancing accuracy and safety.
- Inserting the New Catheter: A new catheter is inserted into the brain’s ventricle. The other end of this catheter is tunneled under the skin, behind the ear, down the neck, and into the abdomen using a technique called subcutaneous tunneling. Additional small incisions along the neck and chest may be made to help guide the catheter.
- Valve Placement: A programmable or fixed-pressure valve is installed and connected to both catheters. The valve regulates fluid flow and ensures drainage only occurs when intracranial pressure exceeds a set threshold.
- Closure and Dressing All incisions are carefully closed with sutures or surgical staples and covered with sterile dressings.
Recovery and Postoperative Care
After surgery, patients are monitored in a recovery room before being transferred to a standard hospital room.
Monitoring includes vital signs, neurological status, and surgical site observation. Imaging may be repeated postoperatively to confirm shunt function and placement.
Short-Term Recovery
Long-Term Outlook
While VP shunt systems are not permanent fixes, many individuals live active and functional lives with properly maintained shunts. Regular check-ups and patient awareness of shunt-related symptoms are vital to long-term success.
Signs Your Shunt May Be Malfunctioning
Knowing the signs of potential shunt failure is critical. Seek immediate medical attention if any of the following occur:
Conclusion
@dr.z_neurosurgery We can this condition hydrocephalus. It can be teeated with a ventriculoperitoneal (VP) shunt or another form if CSF shunting. #vpshunt #hydrocephalus #shunt #neurology #hydrocephaluswarrior #medical #doctor #medtok #neuroscience #brain ♬ original sound – Dr. Z 🧠 Neurosurgery
Ventriculoperitoneal shunt replacement is a vital surgical procedure for individuals with malfunctioning or infected shunt systems. It plays a crucial role in managing hydrocephalus, especially in cases where long-term relief from symptoms is dependent on the continuous drainage of cerebrospinal fluid.
Although shunts can function effectively for years, they are not permanent. Understanding the reasons for replacement, how the procedure is performed, and what to expect during recovery can empower patients and caregivers to make informed decisions and recognize early signs of failure or infection.
With advancements in surgical technique and valve technology, outcomes continue to improve, offering patients a better quality of life and improved neurological function.