Meralgia paresthetica is a condition that causes pain, tingling, burning, or numbness on the outer part of the thigh. Unlike sciatica, this condition does not affect motor control or muscle strength—it solely impacts sensation.
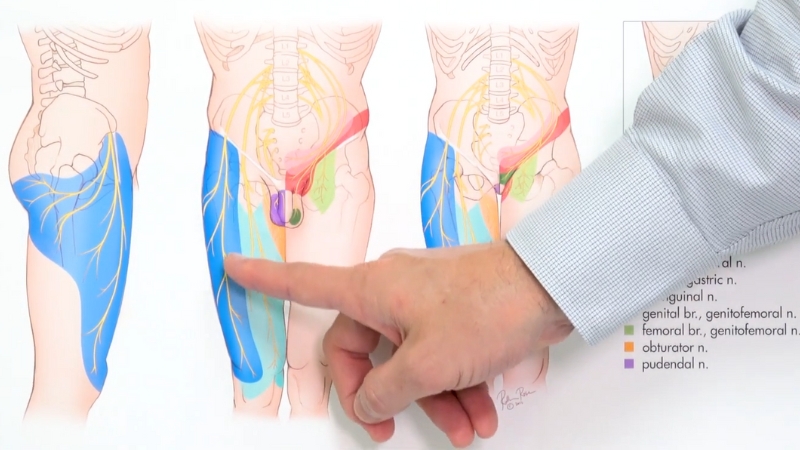
The root cause is the compression or entrapment of a sensory nerve called the lateral femoral cutaneous nerve (LFCN).
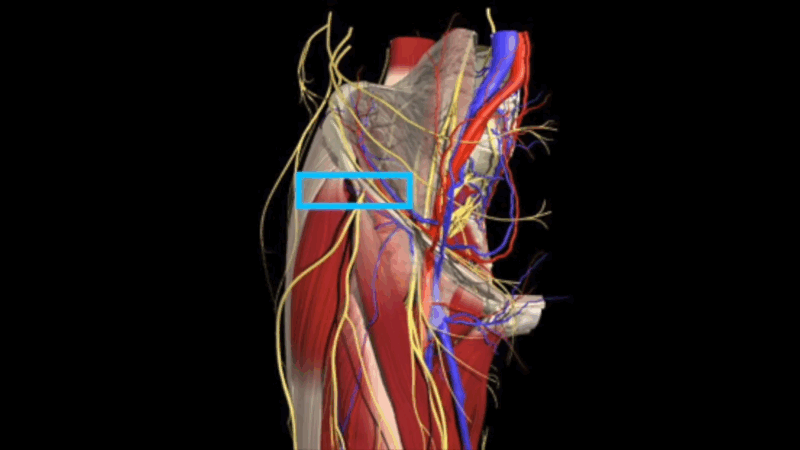
This nerve originates from the lumbar spine (specifically, the L2 and L3 nerve roots), travels through the pelvis, and exits into the upper thigh, passing under or through the inguinal ligament.
When the nerve becomes compressed—often in the region of the anterior superior iliac spine—sensory disturbances occur.
Although meralgia paresthetica is not life-threatening, it can significantly affect quality of life due to chronic discomfort, especially when walking, standing, or wearing certain clothing.
Causes and Risk Factors
There are multiple known causes and risk factors for meralgia paresthetica, most of which are related to increased pressure on the lateral femoral cutaneous nerve. These include:
1. Mechanical Compression
2. Obesity and Weight Gain
Excess body fat can put pressure on the pelvic and groin regions, increasing the likelihood of nerve impingement.
3. Pregnancy
During pregnancy, anatomical changes and increased intra-abdominal pressure can lead to nerve compression.
4. Trauma or Injury
Direct trauma to the pelvic or hip area, such as from falls, accidents, or surgeries (especially orthopedic procedures involving the pelvis or spine), can damage or irritate the nerve.
5. Prolonged Standing or Repetitive Motion
Occupations or activities involving long periods of standing, walking, or repetitive leg movements can increase tension and compression along the nerve’s pathway.
6. Medical Conditions
Symptoms of Meralgia Paresthetica
View this post on Instagram
The hallmark symptoms typically include:
Symptoms are often unilateral (affecting one leg), but in rare cases, they may be bilateral. Pain may worsen with physical activity or prolonged standing and may improve when sitting or reclining.
Diagnosis and Evaluation of Meralgia Paresthetica
Diagnosing meralgia paresthetica requires a careful and methodical approach.
Since this condition arises from compression of the lateral femoral cutaneous nerve, a purely sensory nerve, it must be differentiated from other conditions that might cause similar symptoms, including those involving motor nerves or structural abnormalities in the spine or pelvis.
Medical History Review
The first step in diagnosis involves obtaining a comprehensive medical history. This includes discussing:
Patients often report that discomfort began after a period of wearing tight clothing or belts, following an injury to the hip or pelvis, or during/after pregnancy. These insights help identify lifestyle or mechanical factors contributing to nerve compression.
Physical Examination

The clinician tests sensory responses in the outer thigh using light touch, pinprick, or temperature to identify areas of altered sensation.
Palpation over the anterior superior iliac spine (ASIS) or along the inguinal ligament may reproduce the patient’s symptoms, further indicating nerve involvement.
A basic neurological exam ensures that the motor nerves and reflexes are functioning normally, reinforcing the conclusion that the condition is sensory in nature.
Diagnostic Imaging (Optional)
In many cases, the diagnosis is made clinically, but imaging studies may be used to rule out other structural causes. Common imaging techniques include:
These tools help ensure that other causes of thigh pain or numbness—such as lumbar radiculopathy or pelvic pathology—are excluded.
Electrodiagnostic Testing

If the diagnosis is unclear or if multiple nerve pathways are suspected to be involved, the physician may recommend nerve conduction studies (NCS) and electromyography (EMG). These tests:
Diagnostic Nerve Block
A diagnostic nerve block can serve as both a test and a treatment. In this procedure, a local anesthetic is injected near the lateral femoral cutaneous nerve.
If the patient experiences a rapid and noticeable reduction in symptoms, this strongly suggests that the nerve is the source of pain and confirms the diagnosis of meralgia paresthetica.
This approach not only validates the clinical assessment but also guides the development of a personalized treatment plan. In many cases, patients experience both short-term relief and insight into the potential success of future therapeutic nerve blocks.
Step-by-Step Description of the Procedure
The lateral femoral cutaneous nerve block is a relatively quick and minimally invasive outpatient procedure used to diagnose and treat meralgia paresthetica.
The entire process usually takes less than 30 minutes and involves several well-defined steps to ensure both safety and effectiveness.
Step 1: Patient Positioning
The procedure begins with the patient lying on their back in a relaxed, supported position. The area around the anterior superior iliac spine (ASIS)—near the front of the hip—is exposed.
Proper positioning ensures that the physician can easily access the target site and that the patient remains comfortable throughout the procedure.
Step 2: Skin Preparation
After the patient is positioned, the skin over the targeted area is thoroughly cleansed with an antiseptic solution to minimize the risk of infection.
A sterile drape is placed to maintain a clean procedural field. This step is essential in preventing contamination during the injection.
Step 3: Identification of Landmarks
The physician may palpate key anatomical landmarks to locate the approximate path of the lateral femoral cutaneous nerve.
Since the course of this nerve can vary slightly between individuals, identifying bony and soft tissue references helps in planning accurate needle placement.
Step 4: Imaging Guidance
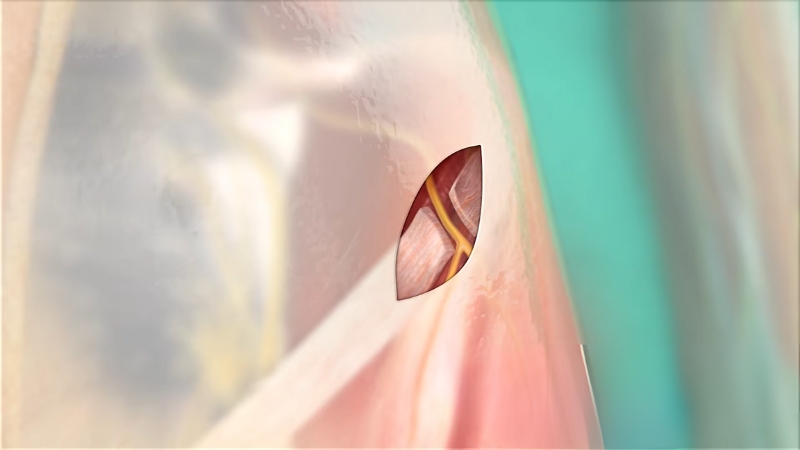
To enhance precision, real-time imaging—typically ultrasound or sometimes fluoroscopy—is used.
This step is especially important because it accounts for individual anatomical variation and improves the success rate of the procedure.
Step 5: Needle Insertion and Injection
Using the imaging for guidance, the physician carefully inserts a fine needle through the skin and advances it toward the nerve. Most patients feel only slight pressure or mild discomfort during this part of the procedure.
Once the needle is confirmed to be near the lateral femoral cutaneous nerve, a mixture of local anesthetic and corticosteroid is slowly injected.
The physician observes the dispersion of the solution on the imaging screen to confirm correct placement.
Step 6: Completion and Dressing
After the injection is completed, the needle is removed, and the injection site is cleaned and covered with a sterile bandage. This protects the area and prevents infection.
Step 7: Monitoring and Discharge
Following the injection, the patient is observed for a short time—usually 15 to 30 minutes—to ensure there are no immediate side effects, such as allergic reactions or unexpected numbness.
Most individuals are able to walk out of the clinic shortly after the procedure and can resume light activities the same day.
Step 8: Post-Procedural Care Instructions
Before leaving, patients are provided with clear post-procedural care guidelines, including:
Following these instructions helps ensure proper healing and maximizes the benefit of the injection.
Bottom Line
@dr.abdulbaker Meralgia paresthetica #meralgia #Nerve #Compression #SCI #backpain #paresthetica #back #lumbar #fracture #fusion #neurosurgery #fyp #viral #lumbarfusion #neurosurgeon #health #physician #wellness #Dallas #Texas #Uae #education #doctor #Disc #medical #spine ♬ original sound – Dr.Baker Brain 🧠 Surgeon
Meralgia paresthetica is a painful and often frustrating condition that stems from compression of the lateral femoral cutaneous nerve, leading to sensory disturbances in the outer thigh. While it is not life-threatening, its symptoms can significantly interfere with daily activities and overall comfort.
Accurate diagnosis begins with a careful clinical evaluation, including a thorough review of medical history, physical examination, and, when necessary, imaging studies or nerve conduction tests.
In many cases, a diagnostic nerve block serves as both a confirmation tool and an effective means of symptom relief.
For individuals who do not experience sufficient relief from conservative treatments, more advanced options, such as intrathecal pain pump placement, may be considered to manage chronic pain.
The lateral femoral cutaneous nerve block is a straightforward, minimally invasive procedure that can offer both immediate and lasting pain relief.
When performed with imaging guidance, it allows for precise targeting of the nerve and minimizes risk. Patients typically tolerate the procedure well and can return to daily activities shortly afterward, with proper care and follow-up.